
What are your child’s personal sleep requirements? Even the experts don’t know for sure.
Sleep has a big impact on our well-being, so it’s understandable that parents want to know if their kids are getting enough. Recent research suggests that something as simple as a well-timed nap makes a difference in how much preschoolers learn (Kurdziel et al 2013). Timely sleep — such as napping no later than 4 hours after learning — helps babies encode new memories (Konrad and Seehagan 2021; DeMasi et al 2021).
But while it’s clear that sleep is important, there is no simple formula for calculating your child’s personal sleep needs. In fact, one of the most striking things about sleep requirements is how little we understand them. The whole notion of “getting enough sleep” may be inherently subjective — dependent on sleep quality, individual physiological factors, and cultural habits (Blunden and Galland 2014; Hunt 2003).
It’s easy to find official-looking sleep charts on the internet. But what data are they based on? Historically, these charts have reflected the results of sleep surveys conducted in Western populations (e.g., Blair et al 2012; Iglowstein et al 2003; Armstrong et al 1994; Roffwarg et al 1966). So they don’t tell us much about how sleep varies across across cultures.
Moreover, surveys sometimes ask people to estimate sleep duration in ways that are bound to be at least a little inaccurate: The resulting numbers may tell us more about how long people spend in bed overnight — not how long they spend actually sleeping.
And of course no chart is going to tell you precisely how much sleep a specific individual needs. Sleep requirements vary from one person to the next.
As the National Center on Sleep Disorders Research has noted, we need large-scale, controlled studies that measure both sleep and biological outcomes (Hunt 2003). Unfortunately, such studies are uncommon.
Notable exceptions are studies focusing on behavior problems and obesity.
For example, a study of 297 Finnish families with children aged 5-6 years, researchers found that kids who slept less than 9 hours each day had 3-5 times the odds of developing attention problems, behavior problems, and other psychiatric symptoms (Paavonen et al 2009).
Another recent study tracked the development of obesity in young children.
In that study, researchers recorded the body weights and sleep habits of kids under five years of age. Then, five years later, they measured the kids again.
The study revealed a link between sleep loss and obesity. Kids who’d gotten less than 10 hours of nighttime sleep at the beginning of the study were twice as likely to become overweight or obese later on (Bell and Zimmerman 2010).
Moreover, researchers found that the timing of sleep mattered. When it came to reducing the risk of obesity, daytime naps didn’t help. For young children, the crucial factor was getting more than 10 hours of sleep at night.
Is the evidence conclusive? No. Some research has failed to find links between sleep time and fat accumulation, like one study of children under the age of 3 (Klingenberg et al 2013), and of course we can’t be sure about causation.
Some kids may suffer from medical conditions that cause both sleep problems and obesity. Perhaps in the near future investigators will resolve these discrepancies.

Meanwhile, how do we know what’s normal?
We can try to answer these questions by consulting the range of sleep times that are typical for many infants, children, and adults (see the tables below).
But keep the following points in mind:
1. There is no optimal number of sleep hours that applies to all adults or all kids (Dement and Vaughan 1999; Jenni et al 2007).
Sleep requirements are probably influenced by growth rates, stress, disease, pregnancy, and other aspects of your physical condition. They may also be influenced by your genes (Gottlieb et al 2007).
2. The most recent scientific study of sleep duration among children reveals a tremendous amount of variation between individuals–especially during early childhood.
For example, newborns may sleep anywhere from 9 to 19 hours a day (Iglowstein et al 2003). Kids at both ends of the spectrum may be healthy and normal.
3.Sleep patterns vary cross-culturally.
In some cases, cultural differences are mostly about the scheduling of sleep.
For instance, in predominantly Asian countries, preschool children get less sleep at night than do kids in predominantly Caucasian countries, but they make up the shortfall by napping during the day (Mindell et al 2013).
In other cases, cultural differences concern the total amount of sleep people get over a 24-hour period.
Kids in China and Italy appear to get less sleep than do children in the Netherlands and the United States (Ottaviano et al 1996; Lui et a 2003; Super et al 1996). Who is better off? At present, we lack scientific studies that address this question (Jenni and O’Connor 2005).
Meanwhile, we shouldn’t assume that the “average sleeper” in any given study is getting the optimal amount of sleep. Some populations may be chronically under-slept; others may be well-rested.
4. In Western countries, recommended sleep durations have changed over time.
For example, in the early 1900s, several sleep experts were advising that toddlers (age 1-2 years) get 17-18 hours of sleep (Matricciani et al 2013).
Today, the National Sleep Foundation says that it’s normal for children in this age group to get 11-14 hours.
Have toddler sleep requirements changed since the 20th century? It seems very unlikely. Official, population-wide recommendations reflect guesswork and cultural norms; they shouldn’t override our personal observations of a child’s energy levels, moods, or signs of fatigue.
5.Too little sleep can have important health consequences.
Scientific studies link childhood sleep loss with fatigue and bad moods (Oginska and Pokorski 2006; Berger et al 2012), attention problems (Fallone et al 2001), impaired memory consolidation (Kurdziel et al 2012), academic problems (Fallone et al 2005), and obesity (Lumeng et al 2007; Bell and Zimmerman 2010).
6. But sleeping less than average isn’t necessarily bad.
Some kids sleep less than others, and they don’t always suffer for it. For example, researchers tracking the sleep habits of Swiss children found that individual differences in sleep time were not correlated with differences in growth. (Jenni et al 2007).
7.Although some parents underestimate how much sleep their children need, others overestimate.
Before imposing any particular sleep schedule on your child, it’s important to determine what your child’s own, individual sleep requirements are. Forcing children to go to bed when they aren’t sleepy can cause bedtime battles and other behavior problems.
What’s typical in the 21st century, English-speaking world?
Clues from a study of British children
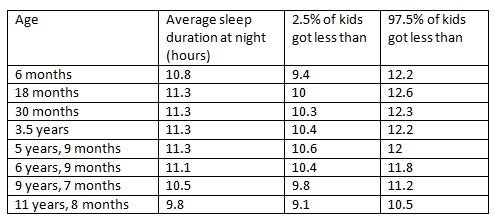
The table below reports the results of a large, prospective study of more than 11,500 kids born in South-West England in 1991-1992.
At 8 different points in time – beginning when the children were 6 months old and ending when they were 11 years old — Peter Blair and his colleagues (2012) asked parents when their kids “normally went to bed in the evening and woke in the morning on an average weekday.”
From these data, the researchers calculated how much time kids spent in bed each night. Because parents rarely know precisely when their children fall asleep or wake up—or how much time kids spend awake in the middle of the night—these parental reports probably overestimate the amount of time kids actually slept (Jenni et al 2007).
The table shows the average nighttime sleep duration for each age group (Blair et al 2012).
It also provides information about the degree of variation. For example, the table indicates that 95% of preschoolers (aged approximately 3.5 years) slept between 10.4 and 12.2 hours. Only 2.5% got less than 10.3 hours, and only 2.5% got more than 12.3 hours.
Note: For more detailed information about baby sleep times, see this article on baby sleep requirements.
What about naps?
The researchers also asked about daytime sleep. Among children who napped, how much time did they log in bed? Here are the results:
- 6 months: 2.4 hours average; range 1.3 – 3.5 hours
- 18 months: 1.5 hours average; range 1 – 2 hours
- 30 months: 1.2 hours average; range 0.7 – 1.7 hours
- 3.5 years: 1.1 hours average; range 0.5 – 1.7 hours
- 5.75 years: 1 hours average; range 0.3 – 1.7 hours
- 6.75 years: 1.2 hours average; range 0.3 – 2.1 hours
Virtually all children 18 months and younger were reported to take naps. Most children (59%) still took naps at the age of 30 months. But by the time kids were 3.5 years of age, only 23% slept during the day, and reports of napping were very uncommon for kids older than 5 years.
The British data are probably consistent with practices in other Northern European and Anglo cultures—-cultures where daytime sleep is discouraged for older children and adults (e.g., Iceland: Thorleifsdottir et al 2002, Switzerland: Iglowstein et al 2003).
But the truth is that human beings are very flexible about when and how they meet their sleep requirements.
In many parts of the world, napping is a normal part of life for children and adults (Worthman and Melby 2002).
In fact, as I noted in my article about night wakings, the historical and anthropological evidence suggests that humans were designed to sleep flexibly (Worthman and Melby 2003; Ekirch 2005).
So the British study is not representative of kids living in “pro-napping” or “siesta” cultures.
For instance, in Saudi Arabia, napping is common among older kids. According to a study of school-age children in Riyadh, 45% of 13-year olds take regular naps (BaHamman et al 2006).
And even in countries where napping is discouraged by the mainstream, specific ethnic groups may encourage napping. In the Southern United States, African-American kids are much more likely to nap—and to nap more frequently—than are European American kids (Crosby et al 2005). In one study, 40% of African-Americans were still taking naps at 8 years of age (Crosby et al 2005).
Is the early abandonment of napping detrimental? For some kids it might be. Recent experimental research indicates that toddlers who skip naps are more likely to (1) show confusion and negative emotion in response to challenging tasks (Berger et al 2012) and (2) have trouble “downloading” new information into long-term memory (Kurdziel et al 2013).
Are kids today meeting their sleep requirements?
The British study tells us about what’s normal among a certain population of children. But what’s normal keeps changing. As the authors note, their results differ substantially from the results of older, earlier studies of Western children.
For instance, a major study of Swiss kids born in the 1970s reported that babies and toddlers got almost an hour more sleep each night than did the more contemporary, British children (Iglowstein et al 2003).
The modern British kids are also falling short of the National Sleep Foundation’s recommendations about sleep requirements (as noted above). And that’s in keeping with an international trend towards shorter sleep times for kids.
From the United States to Saudi Arabia to Hong Kong, recent studies indicate that kids are sleeping less than experts typically recommend (Matricciani et al 2012; BaHammam et al 2006; Ng 2005 Smedje 2007; Tynjala et al 1993).
Is this worrying?
As I note above, it’s hard to say how much sleep the average child needs for optimal health. We need more rigorous, focused research to answer that question.
But given evidence to date that links shorter sleep duration with obesity (mentioned above), attention problems, emotional problems, and impaired academic performance (Vriend et al 2013; Li et al 2013), I think we should be concerned. Some kids may find their personal needs are in-sync with the modern trend towards shorter sleep times. But others may not.
Fine-tuning: Your family’s individualized sleep requirements
Sleep charts may give us a rough idea of what is considered normal. But the best guide to your own sleep requirements is how you feel and perform (Dement and Vaughan 1999). There are several ways to take stock of your individualized sleep requirements-—and the individualized sleep requirements of your kids.
According to Stanford researcher and world-renowned sleep expert William C. Dement, the best way to determine your own sleep requirements is to keep a sleep diary. This involves noting the time you go to bed, the approximate time it takes for you to fall asleep, and the time you awaken in the morning. It also involves keeping track of how sleepy you feel during the day (Dement and Vaughan 1999).
You can adopt this approach for your kids, too. In general, you are probably not getting enough sleep if
- you are sleepy at the wrong time of day (e.g., after waking in the morning);
- you have trouble paying attention during the day,
- you tend to fall asleep very quickly (within a few minutes) when given the chance; or, paradoxically,
- you are “wired” at the wrong time of day (e.g., just before bedtime).
These principles apply to kids, too. Studies reveal other symptoms of sleep deprivation in kids (Dahl 1996), including:
- a child who is easily frustrated and quickly irritated
- a child who has trouble keeping his impulses in check
For more help determining your family’s individualized sleep requirements, click here. You’ll find more details about Dement’s approach, as well as a guide to signs of sleep deprivation in babies and young children.
When you fail to meet your sleep requirements: The health consequences
We may need more rigorous studies about the optimal duration of sleep. But there is no lack of evidence regarding the consequences of severe sleep restriction. In controlled, experimental studies, volunteers assigned to live on very little sleep (typically, 4 hours or less) suffered from the following problems:
- impaired attentiveness (Fallone et al 2001);
- impaired ability to retain new memories (Yoo et al 2007a);
- impaired immune system (Rogers et al 2001);
- greater emotionality (e.g., becoming more upset by disturbing images—Yoo et al 2007b);
- increased afternoon and evening cortisol (stress hormone) levels (Copinschi 2005); and
- increased feelings of hunger (which may lead to overeating—Copinschi 2005).
Other, correlational research hints at long-term problems for people who deviate from the the modern norm.
For example, a study of American adults (ranging from 30-102 years old) showed that people who habitually slept about 7 hours a night had the best survival rates. People who reported either
(1) sleeping less than 6 hours a night, or
(2) sleeping more than 8 hours a night
were more likely to die (Kripke et al 2002).
Interestingly, a separate study of Japanese adults (between 40-79 years of age) had similar results: Sleeping more or less than 7 hours was associated with higher mortality (Tamakoshi and Ohno 2004).
This research got a lot of media attention when it was published, and many headlines implied that there was a causal link between sleep duration and mortality.
But we can’t yet draw any conclusions about causation. As the study authors noted, their research design can’t tell us why people who get more or less sleep are at higher risk. Habitually “short” and “long” sleepers may suffer underlying health problems that cause both sleep disturbances AND increased mortality.
For instance, people with sleep apnea are less efficient sleepers, and may have to sleep longer hours in order to achieve minimal levels of alertness during the day. But sleep apnea patients are also more likely to suffer dangerous health problems, and they are at greater risk of dying while they sleep.
Other life-threatening medical conditions may cause people to sleep longer or shorter than average, resulting in a correlation between long sleep duration and mortality.
The bottom line?
Sleeping more or less than average may be a symptom of an underlying health problem that causes increased mortality. But it may also reflect your perfectly healthy, individually-determined sleep needs. If you habitually sleep much less or much more than average, you might want to have your doctor check you for such health problems as heart disease, sleep apnea, and depression.
References: What scientific studies suggest about human sleep requirements
Armstrong KL, Quinn RA, and Dadds MR. 1994. The sleep patterns of normal children. Med Journal of Australia 161: 202-206.
Ashworth A, Hill CM, Karmiloff-Smith A, and Dimitriou D. 2013. Sleep enhances memory consolidation in children. J Sleep Res. 2013 Dec 16. doi: 10.1111/jsr.12119. [Epub ahead of print]
BaHammam A, Bin Saheed A, Al-Faris E, and Shaihk S. 2006. Sleep duration and its correlates in a sample of Saudi school children. Singapore Medical Journal 47: 875-81.
Barbato G, Barker C, Bender C, et al.1994. Extended sleep in humans in 14 hour nights (LD 10:14): relationship between REM density and spontaneous awakening. Electroencephalogr Clin Neurophysiol. 90:291-297.
Bell JF and Zimmerman FJ. 2010. Shortened Nighttime Sleep Duration in Early Life and Subsequent Childhood Obesity. Arch Pediatr Adolesc Med. 164(9):840-845.
Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. 2012. Acute sleep restriction effects on emotion responses in 30- to 36-month-old children. J Sleep Res. 21(3):235-46.
Blair PS, Humphreys JS, Gringras P, Taheri S, Scott N, Emond A, Henderson J, and Fleming PJ. 2012. Childhood sleep duration and associated demographic characteristics in an English cohort. Sleep ;35(3):353-60.
Blunden S and Galland B. 2014. The complexities of defining optimal sleep: empirical and theoretical considerations with a special emphasis on children. Sleep Med Rev. 18(5):371-8.
Copinschi G. 2005. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmacol. 6(6): 341-347.
Crosby B, LeBourgeois MK, and Harsh J. 2005. Racial differences in reported napping and nocturnal sleep in 2 to 8-year-old children. Pediatrics 115: 225-232.
Dahl RE 1996. The impact of inadequate sleep on children’s daytime cognitive function. Seminars in Pediatric Neurology 3: 44-50
DeMasi A, Horger MN, Allia AM, Scher A, Berger SE. 2021. Nap timing makes a difference: Sleeping sooner rather than later after learning improves infants’ locomotor problem solving. Infant Behav Dev. 65:101652.
Dement W and Vaughan C. 1999. The promise of sleep. New York: Random House.
Ekirch AR. 2005. At Day’s Close: Night in Times Past. New York: WW Norton.
Fallone G, Acebo C, Arnedt JT, Seifer R, and Carskadon MA. 2001. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Mot Skills 93: 213-229.
Fallone G, Acebo C, Seifer R, Carskadon MA. 2005. Experimental restriction of sleep opportunity in children: Effects on teacher ratings. Sleep 28(12): 1561-1567.
Gais S, Lucas B and Born J. 2006. Sleep after learning aids memory recall. Learning and Memory 13: 259-262.
Galland BC, Taylor BJ, Elder DE, Herbison P. 2012. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 16(3):213-22.
Gottlieb DJ, O’Connor GT, and Wilk JB. 2007. Genome-wide association of sleep and circadian phenotypes. BMC Medical Genetics 8(Supplement 1): S9-S16.
Gruber R, Laviolette R, Deluca P, Monson E, Cornish K, and Carrier J. 2010. Short sleep duration is associated with poor performance on IQ measures in healthy school-age children. Sleep Med. 11(3):289-94.
Hunt CE. 2003. National sleep disorders research plan. Bethesda, MD: National Center on Sleep Disorders Research.
Iglowstein I, Jenni OG, Molinari L, Largo RH. 2003. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 111(2): 302-307.
Jenni OG, Molinari L, Caflish JA, and Largo RH. 2007. Sleep Duration From Ages 1 to 10 Years: Variability and Stability in Comparison With Growth. Pediatrics 120(4): e769-e776.
Jenni OG and O’Connor BB. 2005. Children’s sleep: An interplay between culture and biology. Pediatrics 115: 204-215.
Jenni OG, Zinggeler F, Iglowstein I, Molinari L, and Largo RH. 2005. Pediatrics 115(1): 233-240.
Klingenberg L, Christensen LB, Hjorth MF, Zangenberg S, Chaput JP, Sjödin A, Mølgaard C, and Michaelsen KF. 2013. No relation between sleep duration and adiposity indicators in 9-36 months old children: the SKOT cohort. Pediatr Obes. 8(1):e14-8.
Konrad C, Seehagen S. 2021. The effect of napping and nighttime sleep on memory in infants. Adv Child Dev Behav. 60:31-56.
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR 2002. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59:131-136.
Kurdziel L, Duclos K, and Spencer R. 2013. Sleep spindles in midday naps enhance learning in preschool children. PNAS (epub ahead of print) doi: 10.1073/pnas.1306418110.
Kurdziel L, Duclos K, and Spencer R. 2013. Sleep spindles in midday naps enhance learning in preschool children. PNAS (epub ahead of print) doi: 10.1073/pnas.1306418110.
Largo RH and Hunziker UA. 1984. A developmental approach to the management of children with sleep disturbances in the first three years of life. Euro Journal of Pediatrics 142: 170-173.
Lavigne JV, Arend R, Rosenbaum D et al. 1999. Sleep and behavior problems among preschoolers. Journal of Dev Behav Pediatr. 20: 164-169.
Leproult R, Copinschi G, Buxton O, and Van Cauter E. 2007. Sleep loss results in an elevation of cortisol levels the next evening. Sleep 20(10): 865-870.
Li S, Arguelles L, Jiang F, Chen W, Jin X, Yan C, Tian Y, Hong X, Qian C, Zhang J, Wang X, Shen X. 2013. Sleep, school performance, and a school-based intervention among school-aged children: a sleep series study in China. PLoS One. 8(7):e67928.
Lui X, Lui L, and Wang R. 2003. Bed sharing, sleep habits, and sleep problems among Chinese school-aged children. Sleep 26: 839-844.
Lumeng JC, Somashekar D, Appulgliese D, Kaciroti N, Corwyn RF, and Bradley RH. 2007. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics 120: 1020-1020.
Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 129(3):548-56.
Maquet P. 2001. The role of sleep in learning and memory. Science 294: 1048-1052.
Mednick S, Nakayama K, and Stickgold R. 2003. Sleep-dependent learning: a nap is as good as a night. Nature Neuroscience 6: 697-698.
Mindell JA, Sadeh A, Kwon R, Goh DY. 2013. Cross-cultural differences in the sleep of preschool children. Sleep Med. 14(12):1283-9.
Ng DK, Kwok KL, Cheung JM, et al. 2005. Prevalence of sleep problems in Hong Kong primary school children: a community-based telephone survey. Chest 128: 1315-1323.
Oginska H and Pokorski J. 2006. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiol. Int. 23: 1317-1328.
Ottaviano S, Giannotti F, Cortesi F, Bruni O, Ottaviano C. 1996. Sleep characteristics in healthy children from birth to 6 years of age in the urban area of Rome. Sleep 19: 1-3.
Paavonen EJ, Porkka-Heiskanen T, and Lahikainen AR. 2009. Sleep quality, duration and behavioral symptoms among 5-6-year-old children.Eur Child Adolesc Psychiatry. 2009 Dec;18(12):747-54.
Rogers NL, Szuba MP, Staab JP, Evans DL, and Dinges DF. 2001. Neuroimmunologic aspects of sleep and sleep loss. Semin. Clin. Neuropsychiatry 6(4): 295-307.
Roffwarg HP, Muzic JN, and Dement WC. 1966. Ontogenetic development of the human sleep-dream cycle. Science 152: 604-619.
Shur-Fen Gau S. 2006. Prevalence of sleep problems and their association with inattention / hyperactivity among children aged 6-15 in Taiwan. Journal of Sleep Research 5(4): 403-414.
Smedje H. 2007. Australian study of 10- to 15-year olds shows significant decline in sleep duration between 1985 and 2004. Acta Paediatrica 96 (7): 954–955.
Super CM, Harkness S, and van Tijen N. 1996. The three R’s of Dutch childrearing and the socialization of infant arousal. In S. Harkness & C.M. Super (Eds.), Parents’ cultural belief systems: Their origins, expressions, and consequences (pp. 447–466). New York: Guilford Press.
Super CM and Harkness S. 1982. The infant’s niche in rural Kenya and metropolitan America. In: Cross-cultural Research at Issue, pp. 47-55, L.L. Adler (Ed.). New York: Academic Press.
Tamakoshi A and Ohno Y. 2004. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep 27(1):51-4.
Thorleifsdottir , Bjornsson JK, Benediktsdottir B, Gislason T, and Kristbjarnarson H. 2002. Sleep and sleep habits from childhood to young adulthood over a 10- year period. Journal Psychosom Res 53: 529-537.
Toth LA. 2001. Identifying genetic influences on sleep: AN approach to discovering the mechanisms of sleep regulation. Behavior genetics 31: 39-46.
Tynjala J, Kannas L, and Valimaa R. 1993. How young Europeans sleep. Health Educ Res 8: 69-80.
Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers CT, McLaughlin EN. 2013. Manipulating sleep duration alters emotional functioning and cognitive performance in children. J Pediatr Psychol. 2013 Nov;38(10):1058-69.
Worthman CM and Melby M. 2002. Toward a comparative developmental ecology of human sleep. In: Adolescent Sleep Patterns: Biological, Social, and Psychological Influences, M.A. Carskadon, ed. New York: Cambridge University Press, pp. 69-117.
Yoo SS, Gujar N, Hu, Jolesz FA, and Walker MP. 2007a. The human emotional brain without sleep—a prefrontal amygdale disconnect. Current Biology 17(20): 877-878.
Yoo SS, Hu PT, Gujar N, Jolesz FA and Walker MP. 2007b. A deficit in the ability to form new human memories without sleep. Nat Neurosci 10(3): 385-392.
Content of “Sleep requirements” last modified 1/14
Photo credits for sleep requirements article:
image of yawning boy ©iStockphoto.com/Bronwyn8
image of eagle owl ©iStockphoto.com/Dirk Freder